Project Category: Electrical

pIRfusix: Pre-hospital Tissue Perfusion Monitoring
About our project
Motivation
Trauma is the leading cause of death and disability worldwide. The majority of these patients will experience a state of circulatory shock [1] resulting from hemorrhage. This condition can lead to high mortality rates and is characterized by inadequate levels of tissue perfusion. Early, adequate hemodynamic intervention of patients in shock is crucial to prevent worsening organ dysfunction [2]. Tissue perfusion is the measure of oxygen delivery by the blood, which is a way to identify circulatory shock. Commonly used methods of measuring tissue perfusion, such as serum lactate levels, are cumbersome and not always immediately available. Therefore, alternative methods to measure tissue perfusion are needed for early identification of circulatory shock in prehospital patients. Prehospital patient data is invaluable; as it can guide patient care upon arrival by informing the physician about the patient’s status before the patient arrives.
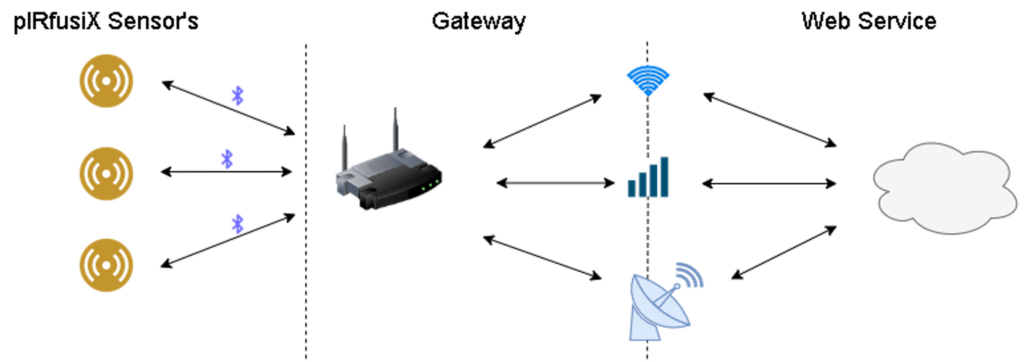
The pIRfusiX system is an IV-pole-mounted communication system leveraging WiFi, 3G cellular networks and the Iridium satellite constellation to provide real-time prehospital localized tissue perfusion patient data to a physician via a web service. The pIRfusiX system consists of wireless custom tissue perfusion sensors performing near infrared spectroscopy (NIRS), a gateway for processing raw tissue perfusion measurements locally, and a web service to visualize and review the tissue perfusion data.
Our Team

Youssef Abdel Maksoud – Full Stack Software Lead

Ryan Ward – Gateway / Communications Lead

Jeff Roszell – Algorithm Lead / Project Manager

Khaled Elmalawany – Sensor Lead

Randy Moore – Sensor PCB Lead
Our Project
HOW OUR DESIGN ADDRESSES PRACTICAL ISSUES
pIRfusiX tackles an ongoing and pervasive issue for pre-hospital care and it’s link to the emergency department at receiving facilities. By relaying vital information about tissue perfusion to the staff at the facility, it gives the department time to respond and increased knowledge of the issues they face when the patient comes through the door.
Discussion with First Responders and EMT determined three key findings:
– The sensor must be unobtrusive
– Must last at least 1 hour (the golden hour in trauma)
– Must provide a metric that is useful and novel
To minimize clutter in the ambulance, we designed our solution to be wireless and modular; the gateway is capable of accepting any Bluetooth connection from commercial devices such as pulse oximeters, paving the way for a wireless sensor suite.
WHAT MAKES OUR DESIGN INNOVATIVE
There are a multitude of disease/injury processes which can be monitored and indicated by a an altered StO2, which is why we chose this metric as the tell tale sign that we wanted to carefully watch and report to the attending physicians and medical staff. As this metric traditionally has no been used in this sense, we intend for pIRfusiX to provide previously unavailable information to the clinicians to help in their decision making. We achieved this through the use of near-infrared light spectroscopy and utilizing a modified beer-lambert equation to track the change in tissue oxygen perfusion.
On top of the unique use of this sensor, we also wanted to make sure that the information could get to the end-user (clinicians at the ER/ICU/Sugery), which is why we integrated multiple communication modules including satellite. This will ensure that the messages can get sent from virtually anywhere in the world. Most related sensors have very little communication standards built-in, therefore this also will give up to date information throughout the patients trip to the facility.
WHAT MAKES OUR DESIGN SOLUTION EFFECTIVE
Careful consideration of the underlying physics of near infrared spectroscopy, input from end users and hospital staff, and laboratory consultation has allowed our solution to be tailored towards usability and functionality. The pIRfusiX system is intended to be applied once to the patient during prehospital transit and follow them throughout their cycle of care. Consultation with hospital staff highlighted that it is common for a patient’s IV-pole to follow them throughout their cycle of care. The pIRfusiX Gateway is an IV-pole mounted hardware, acting as a watchful observer through the patients journey. The wireless sensing of the pIRfusiX combined with its non-invasive readings allows the pIRfusiX system to be easily integrated into existing prehospital-care workflows, creating an effective means of monitoring tissue perfusion.
HOW WE VALIDATED OUR DESIGN SOLUTION
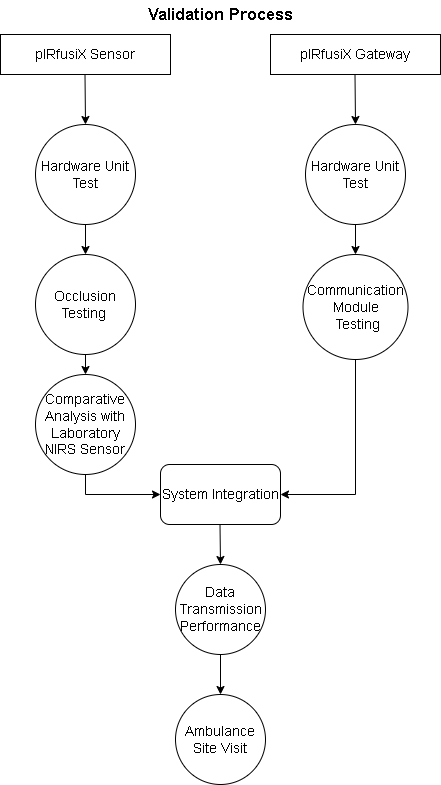
On/Off Battery Normal Performance Testing for Gateway – Allowed for us to that there was no performance loss during handover of power.
Single/Multiple Sensor Normal Performance Testing – Allowed for us to see proper switch off of readings being relayed through the system.
Mild/Moderate/Severe Disruption to Perceived Tissue Perfusion – Allowed for us to see the preciseness and sensitivity of the device as well as determine how severe the stimulus had to be to give us a reading.
Comparison of StO2 Figures with Commercial NIRS Device in Lab -Allowed for validation against already existing standard lab equipment. This made it possible to feel confident in our modified Beer-Lambert equation and its interpretation into code.
WiFi vs Satellite Normal Performance Testing – Allowed for us to meet our standard of being able to send the vital measurements from anywhere a pre-hospital scenario may find itself
Multiple User Web Service Testing – Allowed for the assurance that multiple clinicians could access the details on the web service, as most treatment teams contain members from several disciplines
Loss of Communication Service Testing – Allowed for a guarantee that if the communication was cut, there would be a backup of the information and eventually the measurements would be sent upon a re-established connection
Our Sensor vs. Commercially Available Lab Equipment
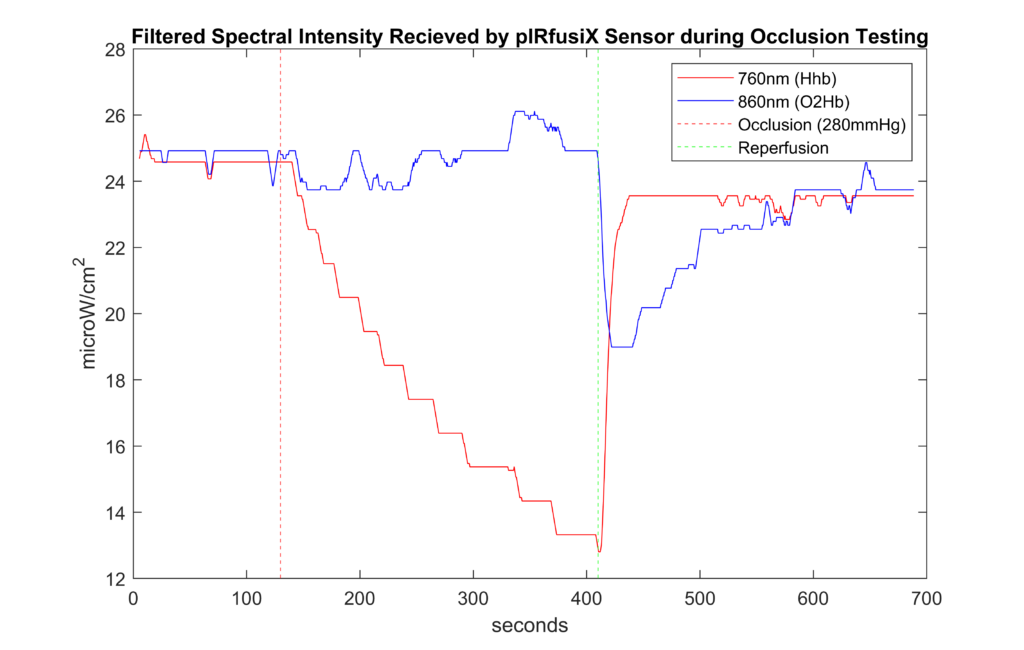
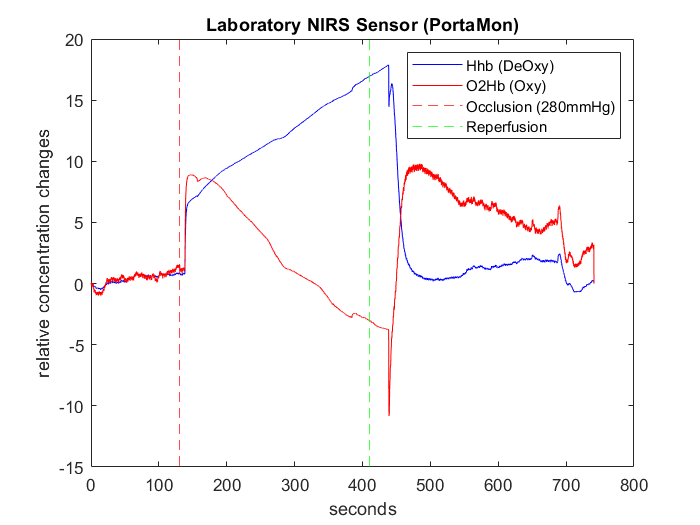
A comparative analysis with a local lab demonstrated the pIRfusiX sensor’s ability to recognize traumatic tissue perfusion events.
FEASIBILITY OF OUR DESIGN SOLUTION
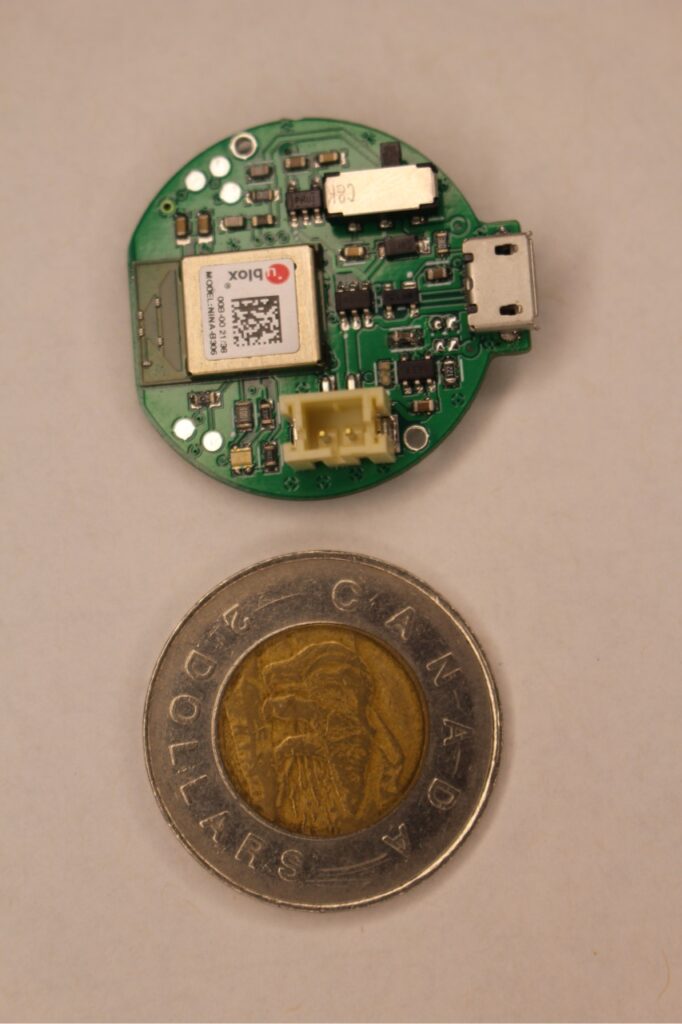
The R&D of the device including multiple revisions of the sensor and multiple prints on the 3D printer for the enclosure came in at $1250 CAD. Now that final measurements and adjustments have been made there could be considerable savings in the manufacturing of the product. Additionally some of the components were chosen not for frugality or performance, but rather on their availability during the pandemic. This led to higher costs on some components. The most expensive and non-negotiable component is the satellite module, however each of the other components could easily have a reduction in cost.
If we look at actual cost to manufacture at our limited scale the cost of a sensor is $50.76 and the gateway is $471.55.
Also another cost we could look at is the cost to transmit one patient worth of data to the web service. By our calculations trips would cost: $122.03 for a Satellite trip and less than $0.10 for a Cellular trip.
Long term the device is not a one time use. The sensor and gateway are meant to be reusable, with the sensor having a replaceable attachment apparatus so it can be kept aseptic for multiple patients. This means that the product is an investment rather than a disposable item.
This paired with the low amount of clinician effort and usefulness of the data it provides, makes pIRfusiX an extremely feasible product to add into the pre-hospital workflow in health services everywhere.
Our Design
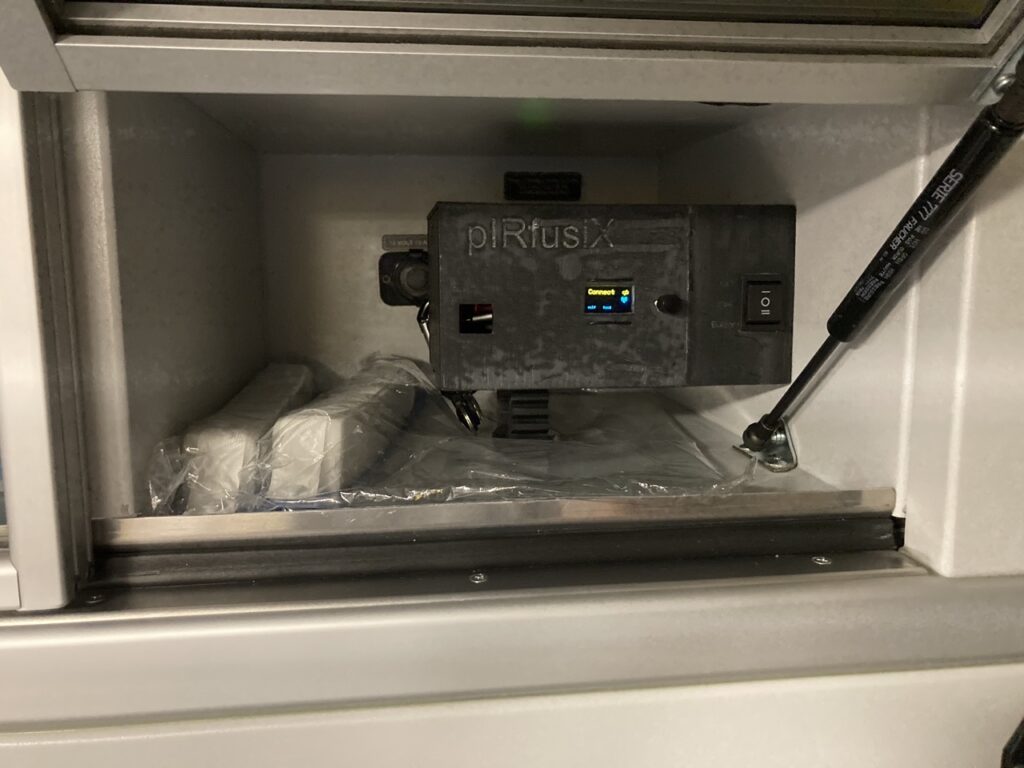
pIRfusiX Gateway
The gateway serves as a midpoint of our system taking in raw data from the pIRfusiX™ sensor, process the data and send it out as StO2 levels the webserver. The purpose of the gateway can be summarized as:
- Collect BLE-transmitted sensor data from the pIRfusiX™ sensor.
- Process raw sensor data to calculate StO2 levels.
- Transmit StO2 values through the appropriate communication modality to the webserver.
- Display StO2 values locally to prehospital personnel
- Store all data locally
The gateway can receive data from the pIRfusiX™ sensor via BLE and then transmit the data via Wi-Fi and Satellite to the webserver. Each represents a different use case, to provide uninterrupted, real-time streaming of sensor data. The satellite is used in remote settings where or where Wi-Fi cannot be received, the Wi-Fi module allows the device to continue to stream data while in a hospital setting (assuming available Wi-Fi).
The gateway receives raw data from the pIRfusiX sensors and processes that data into tissue perfusion measurements then sending the measurements to the webservice. Local processing is done to provide useful information to onsite first responders, while also reducing the amount of data needed to be transmitted over expensive modalities such as satellite.
The Qwiic Iridium 9603n is the satellite transceiver used on the gateway. This is a commercial module, utilizing the Iridium satellite constellation running on the RockBlocks service. The Iridium constellation is a low earth orbit constellation, which was chosen to maximize global coverage and lower latency.
The gateway PCB is enclosed by a 3D printed box which can either be attached to an ambulance via carabiners or attached to an IV pole.


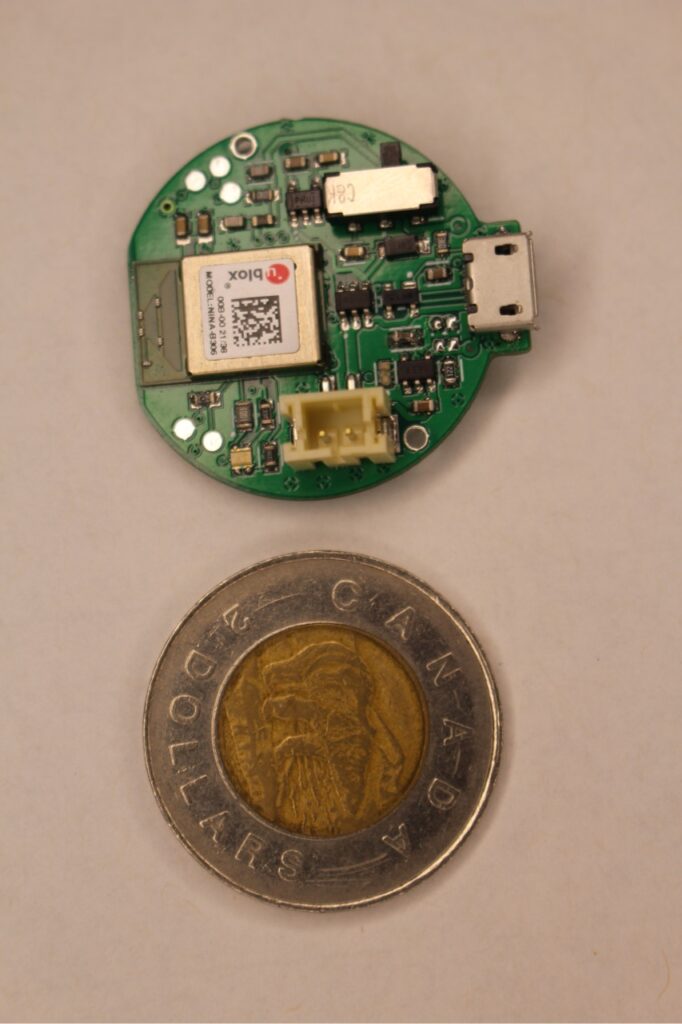
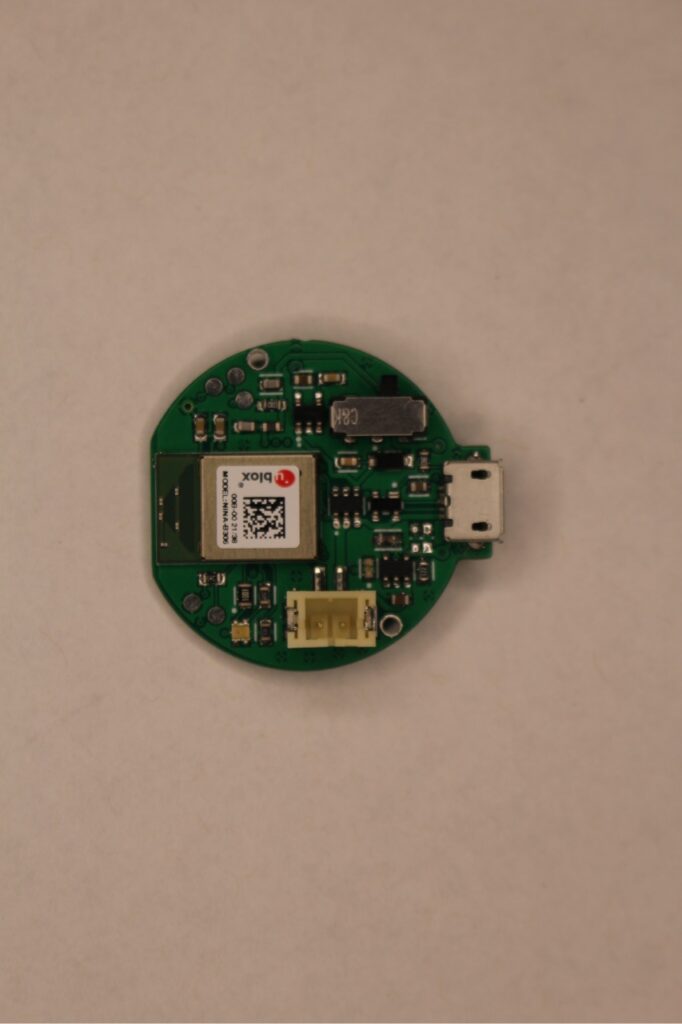
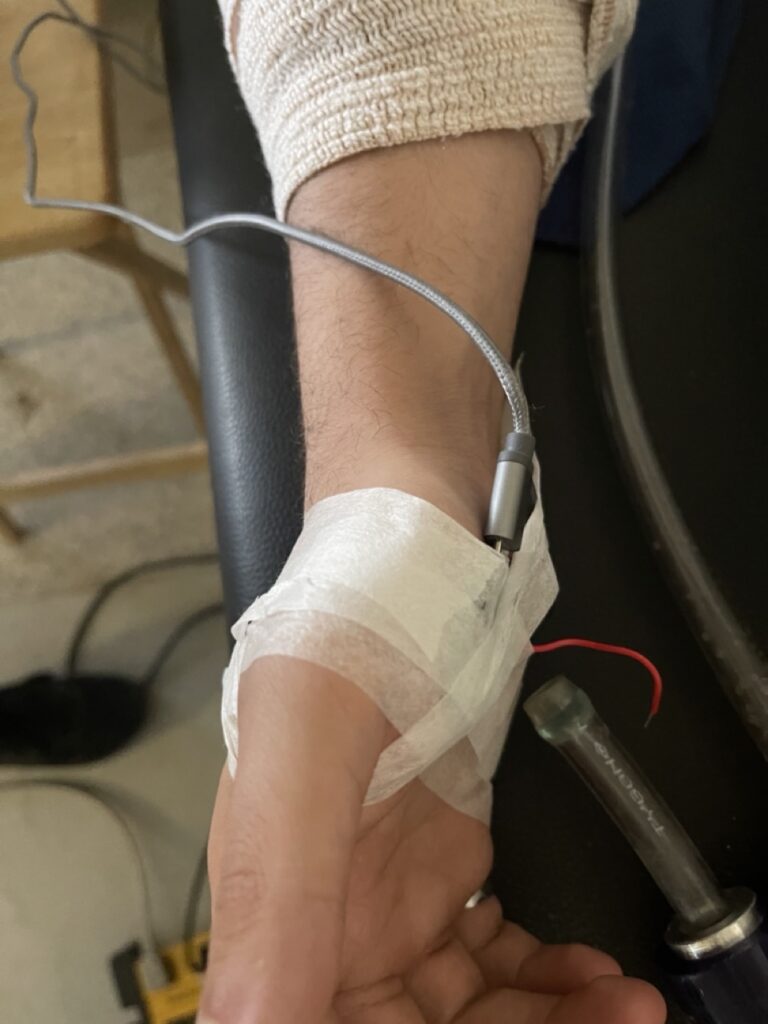
pIRfusX Sensor
The pIRfusiX sensor features a carefully selected microcontroller, the nrf52840: an ultra-low power 2.4 GHz wireless system-on-chip (SOC) integrating a multiprotocol 2.4GHz transceiver and an Arm® Cortex®-M4F CPU. Perfect for low-power, wireless applications, this SOC was selected for its powerful processor and support of the wireless Bluetooth Low Energy protocol. The performance of this chip allowed us the possibility of local analog signal processing as the initial stages of our design involved the simultaneous development of custom near infrared spectroscopy sensors as we validated commercial spectral sensors.
However, preliminary testing of custom near infrared spectroscopy performance did not enable us to detect even drastic tissue perfusion events, such as complete occlusion of blood in a limb.
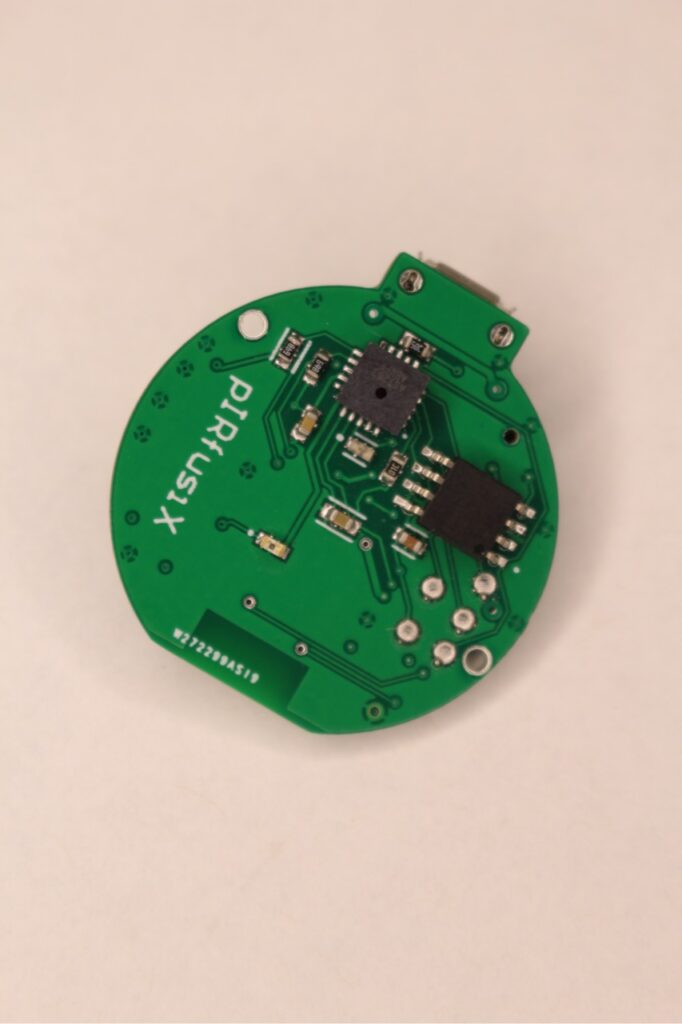
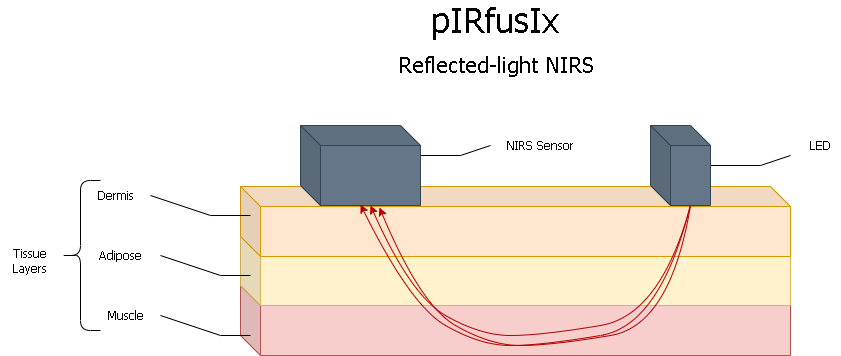
The pIRfusiX sensor performs continuous-wave NIRS on tissue by emitting broadband light on a patient’s skin, ranging from 650nm to 1050nm. Our tissue perfusion measurements are based on fundamental properties of protein species in the blood: oxyhemoglobin (O2Hb) and deoxyhemoglobin (Hhb). Oxyhemoglobin is the oxygen carrying species of hemoglobin found in the blood, while deoxyhemoglobin is the form of hemoglobin without oxygen. Oxyhemoglobin maximally absorbs light at approximately 850nm, while deoxyhemoglobin maximally absorbs light at approximately 775nm. Thus, we designed the pIRfusix sensor to monitor the amount of light absorbed by tissue at these wavelengths to detect changes in how much oxygen is being absorbed by the tissue. To accomplish this task, we selected the AS7263 Spectral Sensing Engine by ams due to its ability to detect light intensity in 6 NIR channels, which include the wavelengths of 760nm and 860nm.
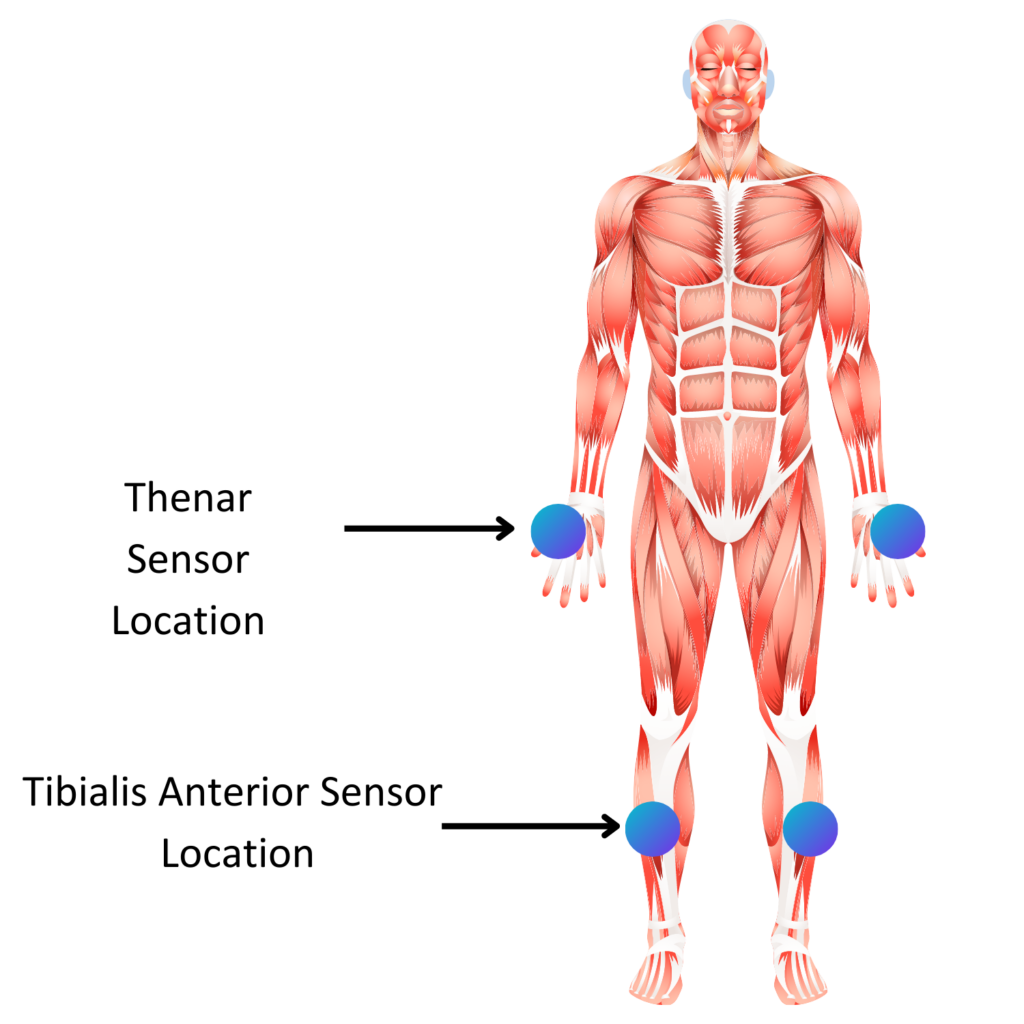
The depth of NIRS plays an important role in sensor performance; too shallow and you will only observe adipose (fat) or skin. To obtain the best possible measurements of peripheral tissue perfusion, we needed to ensure our device targeted the most highly vascularized depth: muscle. Fat thickness underneath the skin varies on individuals, which posed a problem for targeting muscle. However, we designed the pIRfusiX sensors to be small enough to be applied to places on the body where muscle is near the surface, regardless of fat deposits: the thenar region and tibialis anterior region. By careful separation of the LED and spectral sensor, the pIRfusiX sensor targets a depth of 6mm below the skin, which allows us to reach the muscle in the thenar region.
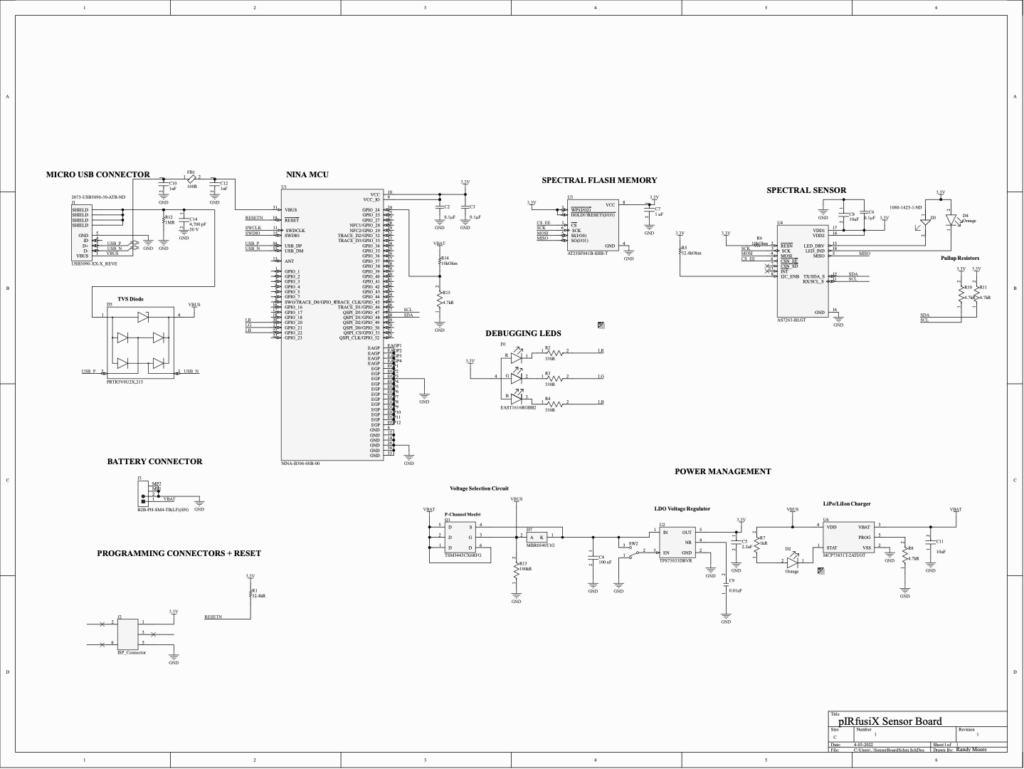
The power management system of the pIRfusiX sensor consists of a simple voltage selection circuit, a linear dropout regulator and a Lithium polymer battery charger.
Power Management
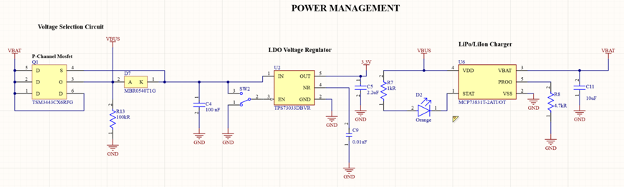
- The voltage selection circuit was implemented to enable both battery powered and outlet-powered operation of the sensor, providing portability but also a long-term monitoring option in hospital.
- The linear voltage regulator was selected to ensure a consistent, noise-free power supply for our sensor system in the presence of the onboard 2.4GHz transceiver. For this, we selected the TPS73033: a low-dropout, high power-supply rejection ratio (PSRR), low noise linear voltage regulator.
- Onboard battery charging for reusability
Sensor System
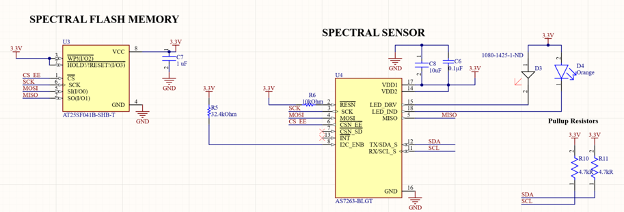
The AS7263 was selected primarily for its NIR channels, but features several attractive features:
- Gaussian optical filters
- Constant-current LED driver
- Electronic shutter control
Algorithm
Modified Beer-Lambert
The pIRfusiX algorithm depends on the Modified Beer-Lambert equation which relates light intensity to a change in concentration of hemoglobin species; protein found in the tissue which carries oxygen.
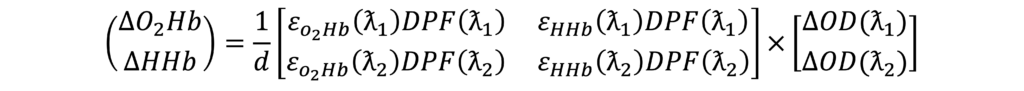
Tissue Perfusion
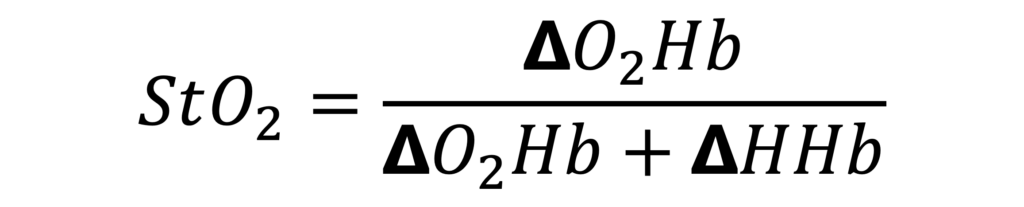
By comparing the amount of light absorbed by oxygenated hemoglobin (02Hb) and deoxygenated hemoglobin (HHb), we can measure the tissue perfusion. This allows a transformation of the data into a percentage of hemoglobin perfused by oxygen, which is our endpoint.
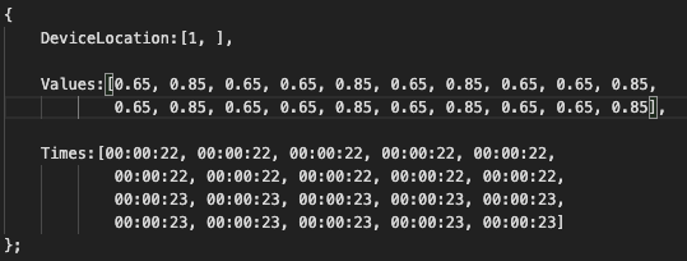
JSON Packaging
Each packaged JSON:
- Which sensor (“DeviceLocation”)
- Latest 20 measurement values
- Timestamps of each measurement
pIRfusiX Web Service
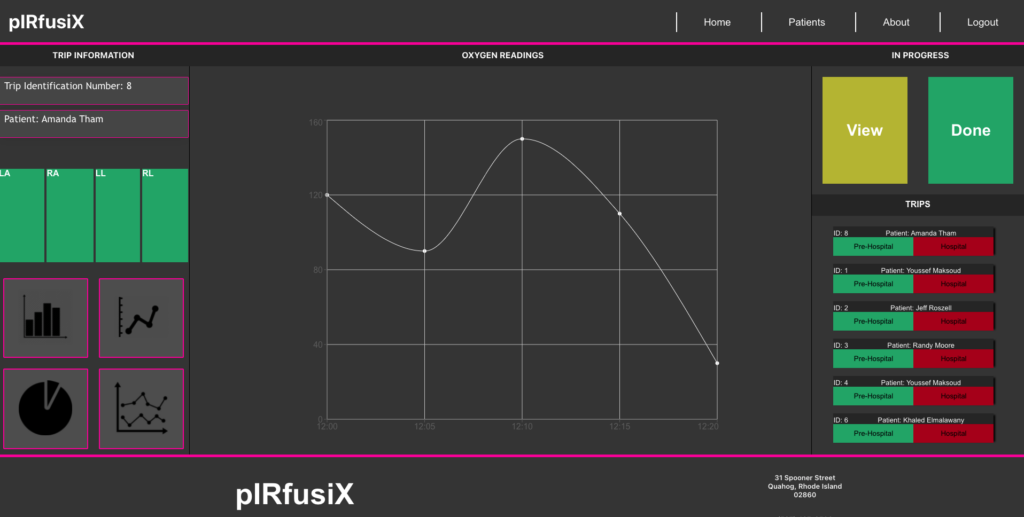
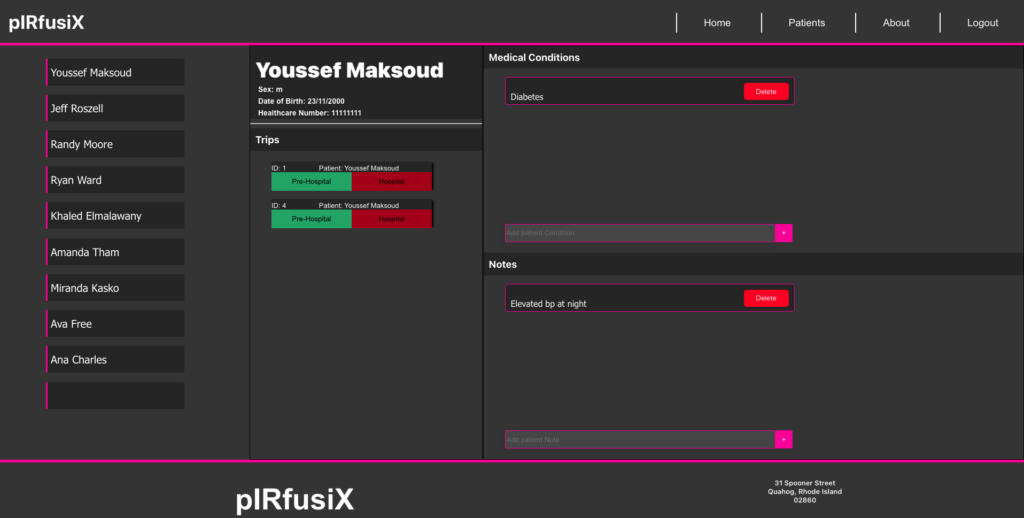
A hosted web service was created using springBoot, REACT, and multiple SQL databases. An API was created to allow for direct HTTP POST messages of the JSON payload to reach the web service. A custom script parses the data into a corresponding database for each of the separate communication standards.
The web service offers:
Authorized Login
Patient Trip Records
Patient Trend Data
Medical Notes
Different Provider Profiles and Access Levels
Automated Entry and Database Retrieval
Real Time Data Display
Heroku was chosen as the hosting service for its flexibility of database compatibility, ease of deployment, and simple pay structure for student projects. There was considerable challenges working within the confines of a low cost(free) framework that was provided by Heroku, however we were able to provide a platform that was capable of reliably delivering a refresh automatically every minute, with on-demand updates available at the clinicians request.
System in Action




Partners and Mentors
pIRfusiX would like to thank:
Our Sponsor
Dr. Paul McBeth for his industry based guidance and biweekly motivational meetings!

Our Academic Advisor
Dr. Kartikeya Murari for his knowledge and insight on the technical side of our project.

Our Teaching Assistant
Zahra Kabirkhoo for her much needed input on the deliverables and continued timeline support.
Academic / Laboratory Professionals
Special thanks to the Dr. Juan Murias and Dr. Letizia Rasica for their input and for allowing us to use their facilities.
References
- Sakr Y, Reinhart K, Vincent JL, Sprung CL, Moreno R, Ranieri VM, De Backer D, Payen D. Does dopamine administration in shock influence outcome? Results of the Sepsis Occurrence in Acutely Ill Patients (SOAP) Study. Crit Care Med. 2006;34:589–597.
- J.-L. Vincent and D. D. Backer, “Circulatory Shock,” The New England Journal of Medicine , vol. 369, pp. 1726-1734, 2013.
